Medical science often encounters scenarios that challenge both its precision and innovation. This blog meticulously unravels the journey of a 73-year-old patient who presented with a complex cardiac condition, highlighting the critical role of advanced diagnostic imaging and collaborative decision-making in achieving optimal outcomes.
Patient Profile and Presenting Complaints
Basic Details:
- Age: 73 years
- Medical History: Diabetes, hypertension
- Condition at Presentation: A three-day-old anterior myocardial infarction (MI)
Clinical Background:
- The patient had moderate left ventricular dysfunction (LVD).
- He had undergone a failed primary percutaneous coronary intervention (PCI) at an outside referral hospital.
These factors combined to make this case one of significant complexity, requiring a multidisciplinary approach and state-of-the-art diagnostic tools to identify the optimal treatment.
Initial Findings and Diagnostic Imaging
Angiographic Results
The patient underwent an angiogram as the first step in evaluating his condition. Key findings included:
- Hazy, eccentric calcific nodules in the Left Main (LM) artery and Proximal Left Circumflex (LCx) artery.
- Angiographic images were unclear and insufficient for precise treatment planning due to the haziness of the lesions.
Angiographic findings in Left Main and LCx arteries.
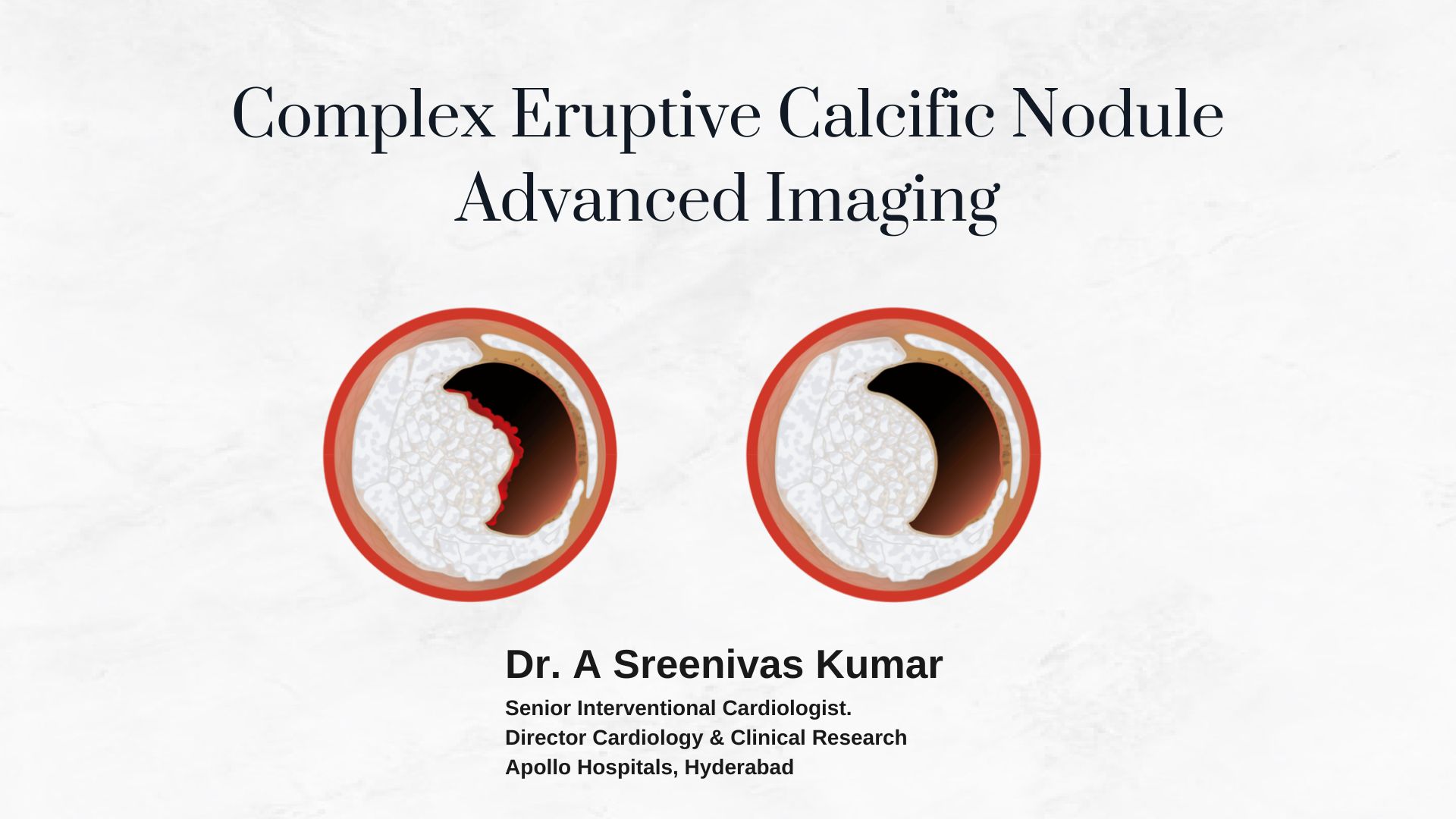
Advanced Imaging: IVUS and OCT
Given the limitations of angiography, the heart team employed Intravascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT) to gain greater clarity.
- IVUS Findings:
- Eruptive calcific nodules were clearly identified in both the Left Main and LCx arteries.
- Cross-sectional images provided critical insights, including the oval shape of the LCx artery lumen.
IVUS imaging highlights eruptive calcific nodules.
- OCT Results:
- OCT offered near-histological resolution, confirming the presence of eruptive calcific nodules in the affected areas.
- It measured the residual LCx area at 5.6 mm², establishing severe stenosis.
OCT imaging provides high-resolution details of calcific nodules.
Clinical Challenges and Decision-Making
This case presented several challenges that complicated treatment planning:
- Total Occlusion:
- The patient’s Proximal Left Anterior Descending (LAD) artery was completely occluded.
- Severe Calcific Disease:
- Both LM and LCx arteries exhibited significant calcification.
- Failed PCI:
- Previous unsuccessful intervention added complexity, increasing the risks associated with repeat PCI.
- Moderate LVD:
- Reduced heart function heightened the risks of any intervention.
The heart team, leveraging the insights from IVUS and OCT, unanimously recommended Coronary Artery Bypass Grafting (CABG) over repeat PCI. CABG was deemed the safer and more effective option, given the patient’s anatomy and clinical history.
The CABG Procedure: A Lifesaving Decision
Coronary Artery Bypass Grafting (CABG) was selected as the treatment of choice for this patient. The procedure aimed to:
- Bypass the Blockages:
Grafts were used to reroute blood flow around the severely calcified lesions. - Reduce Future Risks:
CABG is often associated with better long-term outcomes in cases of severe calcification. - Optimize Cardiac Function:
The procedure aimed to restore adequate blood flow to the heart, potentially improving left ventricular function.
Lessons from This Case
This case holds valuable lessons for interventional cardiology:
1. The Power of Advanced Imaging
- IVUS and OCT are indispensable tools for understanding lesion morphology and severity.
2. The Role of Multidisciplinary Collaboration
- Collaborative efforts among cardiologists, surgeons, and imaging specialists ensure patient-centered care.
3. Tailored Approaches Yield Better Outcomes
- Personalized care, informed by high-resolution imaging, ensures that complex cases receive the best possible treatment.



