
A middle-aged female patient presented with vague chest pain and non-specific complaints. This seemingly benign presentation masked potential underlying coronary artery disease (CAD). The ECG demonstrated T wave inversion in leads V1-V4, raising suspicion of myocardial ischemia. However, an echocardiogram conducted subsequently was unremarkable, with no evident structural or functional abnormalities.
This diagnostic uncertainty led the patient to undergo coronary angiography at another facility, where an angiographic lesion was identified. She was referred for percutaneous coronary intervention (PCI). However, the ostial location of the lesion, its proximity to a ramus, and the apparent size discrepancies between the left main coronary artery (LM) and the left anterior descending artery (LAD) raised questions about the severity of the lesion. To clarify these uncertainties, Optical Coherence Tomography (OCT) and Fractional Flow Reserve (FFR) assessments were performed.
Clinical Background and Initial Evaluation
Patient Presentation:
- Age and Gender: Middle-aged female
- Symptoms: Vague chest pain and non-specific complaints
Initial Investigations:
- ECG Findings: T wave inversion in leads V1-V4
- Echocardiogram: Normal findings, ruling out significant structural abnormalities
- Coronary Angiogram: Identified lesion but with unclear severity, leading to referral for further evaluation.
The diagnostic pathway exemplifies the challenge in evaluating intermediate coronary lesions, especially in patients with non-specific symptoms. To guide treatment effectively, an accurate functional assessment of the lesion’s impact on myocardial blood flow is essential.
Diagnostic Tools: OCT and FFR
Optical Coherence Tomography (OCT):
OCT provides high-resolution intravascular imaging, enabling precise characterization of coronary lesions. In this case, OCT revealed a minimal luminal area (MLA) of 3.2 mm². An MLA greater than 3 mm² is often associated with functionally non-significant stenosis, corroborating the subsequent FFR findings.
OCT Key Findings:
- Smallest luminal area: 3.2 mm²
- The lesion’s ostial location required meticulous imaging to avoid overlooking functional implications.
Fractional Flow Reserve (FFR):
FFR measures the pressure difference across a coronary lesion during hyperemia, providing a functional assessment of its significance. An FFR value greater than 0.80 is considered non-significant for ischemia.
FFR Results:
- Pa (Aortic Pressure): 94 mmHg
- Pd (Distal Coronary Pressure): 88 mmHg
- FFR: 0.93 (Negative)
The negative FFR further reinforced the conclusion that the lesion was unlikely to cause ischemia, negating the need for PCI and favoring medical management.
Management Decision
Given the findings from OCT and FFR, the decision was made to pursue aggressive medical management rather than PCI. This approach was based on the following considerations:
- MLA > 3 mm²: Suggestive of adequate luminal area for coronary blood flow.
- Negative FFR: Functional assessment indicated no significant flow limitation.
- Lesion Complexity: The ostial location and proximity to a ramus posed a higher risk for complications if PCI were attempted.
- Patient Stability: Absence of overt ischemia or unstable symptoms supported a conservative approach.
Case Implications
This case highlights the critical role of advanced diagnostic modalities in guiding the management of intermediate coronary lesions. Without OCT and FFR, the patient might have been subjected to unnecessary PCI, with its attendant risks and costs.
Key Takeaways:
- MLA > 3 mm² generally correlates with a negative FFR, suggesting that medical therapy is sufficient in such cases.
- In challenging cases involving ostial lesions and adjacent branches, functional assessment (FFR) provides invaluable guidance.
- A conservative approach often mitigates risks associated with intervention while ensuring patient safety.
Images and Their Importance
FFR Recording
This image demonstrates the FFR measurement process. The aortic pressure (Pa) and distal coronary pressure (Pd) are shown, along with the calculated FFR value of 0.93, confirming a non-significant lesion.
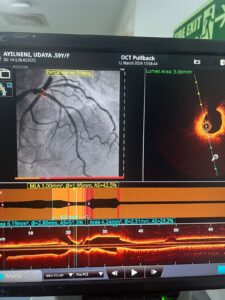
OCT Pullback
The OCT imaging highlights the smallest luminal area of 3.2 mm², visually confirming sufficient coronary lumen to maintain blood flow.
Annotated Coronary Angiogram
The angiographic image emphasizes the ostial lesion’s location and its proximity to a ramus branch, underscoring the complexity of intervention.




FAQs
1. What is the role of OCT in assessing coronary lesions? OCT provides high-resolution imaging to evaluate the size and characteristics of coronary lesions. It helps in determining the minimal luminal area (MLA), which correlates with the lesion’s functional significance.
2. What does a negative FFR indicate? A negative FFR (value > 0.80) suggests that the lesion is not functionally significant, meaning it does not cause a substantial reduction in blood flow to the myocardium.
3. Why was PCI not performed in this case? PCI was avoided because both OCT and FFR indicated that the lesion was non-significant. Additionally, the lesion’s ostial location and proximity to adjacent branches posed a higher risk for procedural complications.
4. What is the significance of an MLA greater than 3 mm²? An MLA > 3 mm² typically correlates with a negative FFR, suggesting that the lesion does not cause significant blood flow limitation and can be managed conservatively.
5. When should OCT and FFR be used together? OCT and FFR are complementary tools often used in intermediate lesions or complex scenarios, such as ostial lesions, to combine anatomical and functional assessments for optimal decision-making.
6. Can medical therapy alone manage significant coronary lesions? While medical therapy is effective for non-significant lesions (as in this case), significant lesions with positive FFR values often require revascularization, either via PCI or coronary artery bypass grafting (CABG).
7. What are the risks of unnecessary PCI? Unnecessary PCI can lead to complications such as stent thrombosis, restenosis, vessel injury, and increased healthcare costs without providing additional clinical benefit.



